Overview & Epidemiology
- Uncommon but serious allergic eye condition.
- Affects children and young adults:
- Onset: 5–15 years
- Duration: 5–10 years
- Onset: 5–15 years
- Sex predilection:
- More common in males before puberty
- No gender bias after puberty
- More common in males before puberty
- Ethnic & Geographic trends:
- Decreasing among Caucasians
- Increasing among South Asians
- Tarsal/palpebral form → more common in pale-skinned Caucasians
- Limbal form → more common in darker-skinned individuals
- Often presents as a mixed form
- More common in warm climates
- Typically seasonal: Spring/Summer
- Decreasing among Caucasians
- Atopic association:
- 80% of patients have a history of atopy
- Immune mechanism:
- Type I hypersensitivity
- Cell-mediated immunity (Th2 dominant)
- Th2 cytokines inhibit matrix metalloproteinases (MMPs), leading to collagen build-up in conjunctiva
- Type I hypersensitivity
- 80% of patients have a history of atopy
👁️ Clinical Features
- Typical presentation:
- Young male, spring season, history of atopy
- Symptoms: Intense itching, thick ropy mucus discharge
- Young male, spring season, history of atopy
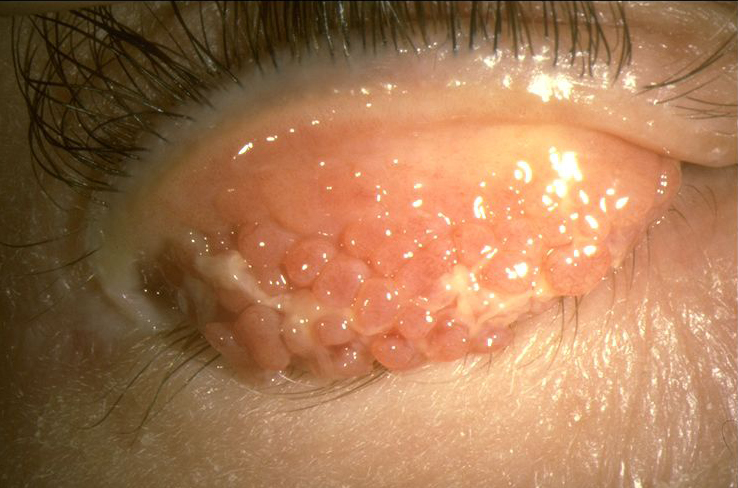
- Tarsal Signs:
Flat-topped giant papillae (“cobblestone appearance”) on upper tarsal conjunctiva
- Limbal Signs:
- Limbal papillae
- Trantas dots: white dots at limbus (aggregates of eosinophils)
- Limbal papillae
- Corneal Involvement (Keratitis):
- Superior punctate epithelial erosions
- Vernal shield ulcer with adherent mucus plaque
- Can lead to subepithelial scarring
- Can lead to subepithelial scarring
- Pseudogerontoxon: lipid deposition near limbus
- Superior punctate epithelial erosions
🧬 Overview & Epidemiology
- Uncommon but serious allergic eye condition.
- Affects children and young adults:
- Onset: 5–15 years
- Duration: 5–10 years
- Onset: 5–15 years
- Sex predilection:
- More common in males before puberty
- No gender bias after puberty
- More common in males before puberty
- Ethnic & Geographic trends:
- Decreasing among Caucasians
- Increasing among South Asians
- Tarsal/palpebral form → more common in pale-skinned Caucasians
- Limbal form → more common in darker-skinned individuals
- Often presents as a mixed form
- More common in warm climates
- Typically seasonal: Spring/Summer
- Decreasing among Caucasians
- Atopic association:
- 80% of patients have a history of atopy
- Immune mechanism:
- Type I hypersensitivity
- Cell-mediated immunity (Th2 dominant)
- Th2 cytokines inhibit matrix metalloproteinases (MMPs), leading to collagen build-up in conjunctiva
- Type I hypersensitivity
- 80% of patients have a history of atopy
👁️ Clinical Features
💊 Treatment
🔸 Topical Treatment
- Mast Cell Stabilizers:
- Sodium cromoglicate 2%, 4×/day
- Sodium cromoglicate 2%, 4×/day
- Topical Steroids:
- For acute exacerbations:
- Dexamethasone 0.1% PF, hourly
- Dexamethasone 0.1% PF, hourly
- Taper to maintenance:
- Fluorometholone 0.1%, 1–2×/day
- Fluorometholone 0.1%, 1–2×/day
- Use lowest effective dose to reduce side effects
- For acute exacerbations:
- Topical Ciclosporin (steroid-sparing):
- 0.1% ciclosporin drops, 3–4×/day (unlicensed)
- 0.2% ciclosporin ointment, 3–4×/day (off-label; veterinary-licensed)
- Can be used long-term to reduce steroid dependence
- 0.1% ciclosporin drops, 3–4×/day (unlicensed)
- Injectable Steroids –
Agent:Triamcinolone acetonide 40 mg/mL
Dose: 0.5–1 mL via posterior sub-Tenon’s injection
- Sunconjunctival
- Subtenons
- Subtarsal
- Mucolytics (for thick mucus plaques):
- Acetylcysteine 5%, 4×/day
- Acetylcysteine 10% PF, 4×/day (hospital special preparation)
- Acetylcysteine 5%, 4×/day
🔸 Systemic Treatment
- Consider systemic immunosuppression in severe/refractory cases
- Collaborate with a dermatologist or clinical immunologist
- Collaborate with a dermatologist or clinical immunologist
- If immunosuppressants used → Herpes prophylaxis required:
- Aciclovir 200 mg 5×/day or 400 mg 2×/day
- Aciclovir 200 mg 5×/day or 400 mg 2×/day
🔸 Surgical Management
- For persistent plaques or shield ulcers:
- Debridement
- Superficial lamellar keratectomy
- Debridement
Also refer, https://eyewiki.org/Vernal_Keratoconjunctivitis