Author: Dr. Hemali Kanabar
The early detection of keratoconus—especially in patients seeking refractive surgery—is critical. One of the most powerful diagnostic tools at our disposal is the Pentacam, a rotating Scheimpflug imaging system that gives a complete 3D view of the anterior segment. But how do you really read a Pentacam? And what are its limitations?
This guide breaks it down for you.
🔷 What is Pentacam?
The Pentacam (Oculus) uses a rotating Scheimpflug camera to capture thousands of cross-sectional images of the cornea, anterior chamber, and lens in under 2 seconds. It generates comprehensive maps of:
- Anterior & posterior corneal curvature (topography)
- Anterior & posterior elevation
- Corneal thickness (pachymetry)
- Anterior chamber metrics (depth, volume, angle)
- Belin/Ambrosio Enhanced Ectasia Display (BAD-D)
It’s especially powerful because it images the posterior corneal surface, which is where ectasia often begins.
🔍 How to Read a Pentacam: Step-by-Step
Think of Pentacam interpretation like assembling a puzzle. Here’s a structured method:
1. Curvature (Sagittal) Map – “Shape and Symmetry”
- Colors: Blue = flatter, Red = steeper
- Look for asymmetry, especially inferior steepening.
- A symmetric bow-tie is normal.
- An asymmetric bow-tie, especially with inferior or inferotemporal steepening, raises suspicion for keratoconus.
- SRAX (skewed radial axis): rotation between superior and inferior hemimeridians.
2. Elevation Maps – “What’s Poking Out?”
These maps compare the cornea to a best-fit shape (sphere or toric ellipsoid):
🔸 Anterior Elevation
- Normally smooth and within ±10 µm
- Elevation > 8–12 µm is suspicious
🔸 Posterior Elevation
- More sensitive for early disease
- Elevation > 15–20 µm is highly suggestive of keratoconus
3. Pachymetry Map – “Where’s the Thinnest Point?”
- Normal cornea: Centrally thin (~540–550 µm) and thickens peripherally in a regular pattern
- Keratoconus: Thinnest point is < 500 µm, often decentered inferotemporally
- Look for:
- Pachymetric Progression Index (PPI) – measures how rapidly thickness increases peripherally
- Ambrósio Relational Thickness (ARTmax) – combines thickness and rate of change; values < 339 µm are suspicious
4. Belin/Ambrosio Enhanced Ectasia Display (BAD-D) – “The Summary Score”
This powerful composite tool integrates:
- Anterior elevation deviation (Df)
- Posterior elevation deviation (Db)
- Pachymetric progression (Dp)
- Thinnest point displacement (Dt)
- Relational thickness (Da)
🔹 BAD-D Score:
- < 1.6 = normal
- 1.6–2.6 = suspicious
- 2.6 = abnormal
This is especially helpful when individual maps are borderline.
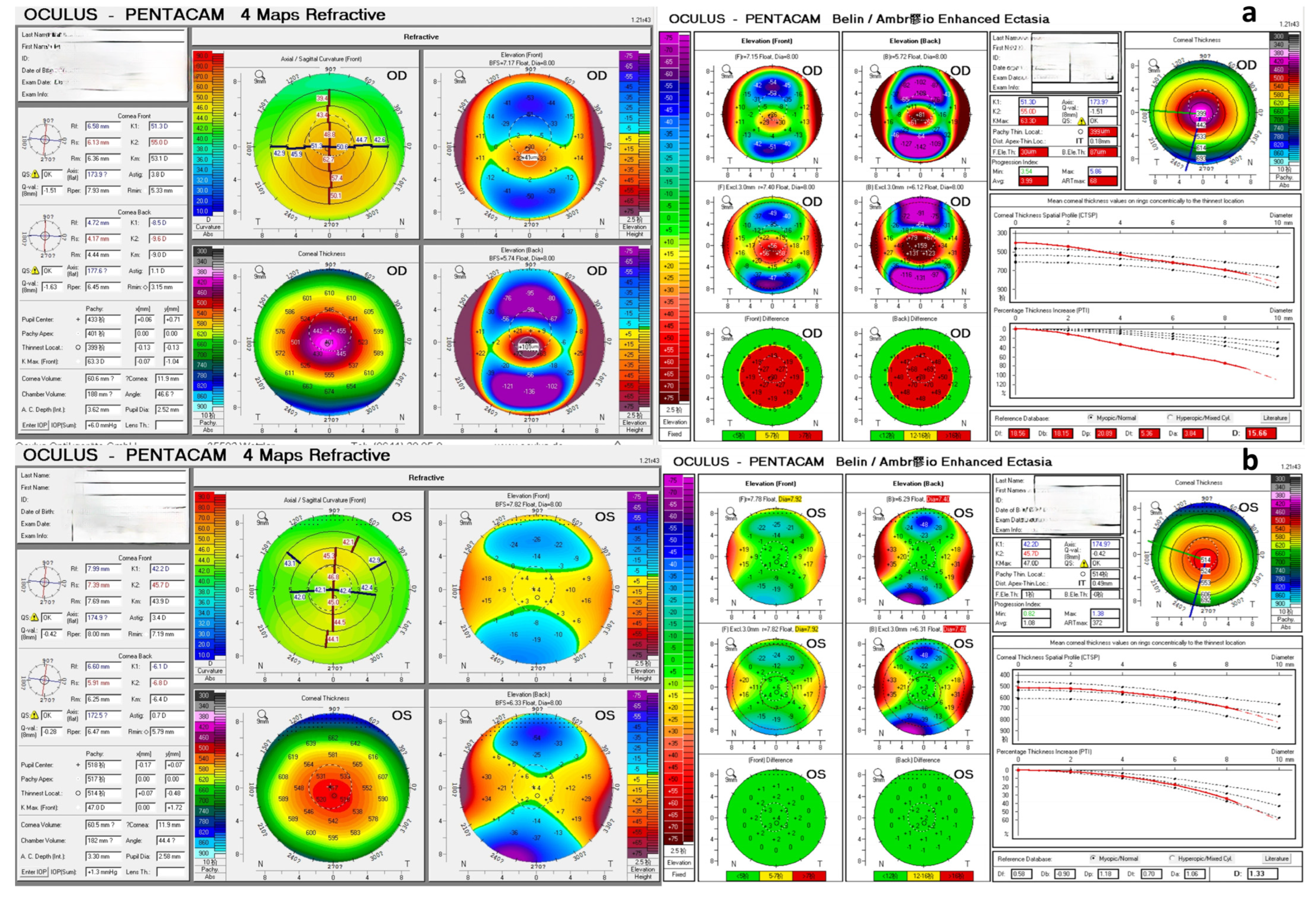
✅ Checklist for Early Keratoconus on Pentacam
| Parameter | Suspicious Value |
|---|---|
| Anterior elevation (BFTE) | > 8–12 µm |
| Posterior elevation | > 15–20 µm |
| Thinnest pachymetry | < 500 µm |
| Thinnest point location | Inferotemporal |
| ARTmax | < 339 µm |
| BAD-D score | > 2.6 |
🧠 Pentacam in Keratoconus: Clinical Relevance
- Detects subclinical or forme fruste keratoconus
- Helps monitor disease progression over time
- Contraindicates LASIK in patients with early signs of ectasia
- Useful in planning crosslinking, specialty contact lenses, or ICRS
⚠️ Limitations of Pentacam
No technology is perfect. Here are key limitations to be aware of:
1. Dependent on Scan Quality
- Artefacts from blinking, poor fixation, dry eyes, or poor tear film can distort results
- Always check the Quality Specification Bar before interpreting data
2. False Positives in Thin Corneas
- Physiologically thin corneas (e.g., in Indian or South Asian populations) can show borderline readings
- Interpretation should always consider clinical findings
3. Lack of Standard Reference in Children
- Pediatric eyes may have slightly different corneal curvature and pachymetry distributions
4. BAD-D Score Not Diagnostic Alone
- It’s a screening tool, not a stand-alone diagnostic criterion
- Always integrate it with clinical signs and individual maps
5. Cannot Directly Diagnose Acute Hydrops or Scarring
- Structural anomalies like stromal scars or hydrops may distort the maps and make interpretation challenging
📝 Final Thoughts
The Pentacam is an incredibly powerful tool when understood correctly. Instead of relying solely on one index, approach it like a detective—correlate:
- Shape (Curvature)
- Elevation
- Thickness pattern
- Composite scores
- And most importantly, the clinical context
If you’re an ophthalmology trainee or FRCOphth aspirant, mastering this device is a must—not just for exams, but for real-world patient safety.
📢 Coming Soon:
Case-based Pentacam interpretation series – real scans, real decision-making. Stay tuned!