By Dr. Hemali Kanabar | Ophthalmology Insights
Salzmann Nodular Degeneration (SND) might not be the most common topic in daily ophthalmic practice, but for the seasoned clinician or FRCOphth candidate, it’s an essential entity to recognize. Subtle in appearance yet significant in impact, SND is a classic example of how chronic ocular surface stress can manifest in the corneal stroma.
Let’s unpack this condition from pathogenesis to management, with clinical pearls along the way.
👁️ What Is Salzmann Nodular Degeneration?
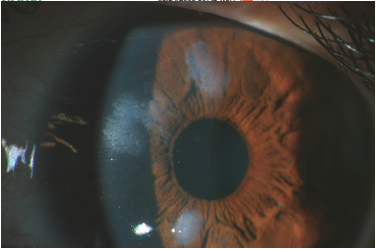
SND is a non-inflammatory, slowly progressive degenerative condition of the cornea, characterized by elevated bluish-white subepithelial nodules, typically located in the mid-peripheral to peripheral cornea. These nodules are often bilateral and more commonly seen in middle-aged to elderly women.
🔬 Pathophysiology
The exact etiology is not fully understood, but SND is thought to result from:
- Chronic ocular surface irritation or inflammation
- Disruption in epithelial-stromal interactions
- Abnormal extracellular matrix deposition and Bowman’s layer replacement by fibrous tissue
It may occur idiopathically or secondary to:
- Dry eye disease
- Meibomian gland dysfunction
- Chronic blepharitis
- Previous trauma or surgery (e.g., LASIK, PK)
- Inflammatory conditions like vernal or atopic keratoconjunctivitis
🔎 Clinical Features
- Nodules: Elevated, bluish-white to grey nodules, 1–2 mm in size
- Location: Superficial stroma, beneath an intact epithelium, commonly in the mid-peripheral cornea (between 3 and 9 o’clock positions)
- Symptoms:
- Often asymptomatic
- May present with foreign body sensation, glare, or reduced vision if nodules encroach upon the visual axis
🧪 Diagnostic Tools
- Slit-lamp biomicroscopy: Key for identifying the nodules
- Anterior Segment OCT: Shows hyperreflective subepithelial lesions
- Topography: May reveal irregular astigmatism or localized flattening
- Histology (if excised): Absence of Bowman’s layer with subepithelial fibrosis and hyaline degeneration
🛠️ Differential Diagnoses
- Band keratopathy
- Salzmann’s degeneration vs. spheroidal degeneration
- Nodular episcleritis or phlyctenulosis (if adjacent to limbus)
- Intraepithelial neoplasia (very different clinically, but worth ruling out)
💊 Management Options
Conservative
- Lubricants (preservative-free)
- Lid hygiene and MGD management
- Anti-inflammatory drops: Mild topical steroids or cyclosporine in selected cases
- Treat underlying surface disease (e.g., blepharitis, VKC)
Surgical
Indicated when vision is affected or nodules are symptomatic:
- Superficial Keratectomy (SK): Mainstay for central nodules or visual symptoms
- Phototherapeutic Keratectomy (PTK): Improves surface smoothness and vision
- Lamellar or Penetrating Keratoplasty: Rarely needed
⏳ Prognosis and Recurrence
- Visual prognosis is generally good after SK or PTK
- Recurrence is possible, especially if the underlying cause is not addressed
- Long-term ocular surface management is key to preventing recurrence
📝 FRCOphth Tip
Salzmann’s nodular degeneration may feature in ocular surface disorders, external eye disease, or even as a subtle image-based station. If a clinical photo shows elevated nodules in an elderly patient with dry eye or rosacea history—think SND!
Don’t forget: management includes not just removing the nodules but also treating the surface disease that led to them.
📚 Suggested Reading
- Krachmer et al. Cornea textbook
- Review articles in BJO or Eye Journal
- Anterior segment OCT case series
💬 Final Thoughts
Salzmann Nodular Degeneration is a reminder that even non-inflammatory conditions can affect vision and quality of life. A good ophthalmologist doesn’t just remove the nodules—they investigate and address the root cause. That’s the art of practice—and the heart of our exams.